Insomnia: a ticking clock for depression?
First created | 05/12/2009
Last edited |
The association between insomnia and depression has been reported countless times. In clinical studies with depressive patients, insomnia was reported to be as frequent as 60%.
Insomnia can be the main complaint for consultation, a prodromal symptom, an early indicator of relapse into depression, or a residual symptom. Why so much emphasis on insomnia? Epidemiologic studies have consistently shown that between 10% and 20% of individuals complaining of insomnia had depression.
Similarly, retrospective studies that examined whether the insomnia resulted from a sleep disorder or was a symptom of a mental disorder have demonstrated that insomnia is mostly an associated symptom of the mental disorder and does not warrant a separate diagnosis of insomnia (Ohayon, 1997).
However, how the chronicity of insomnia affects this relationship and how often chronic insomniac subjects have previously suffered from a mental disorder has been only minimally investigated. Results from longitudinal studies have revealed that individuals with insomnia at the first assessment were more likely to develop a depressive disorder at the second assessment and the persistence of insomnia problems over the time increased the likelihood of developing a concomitant mental disorder (Breslau et al., 1996; Ford and Kamerow, 1989; Roberts et al., 2000; Perlis et al., 2006).
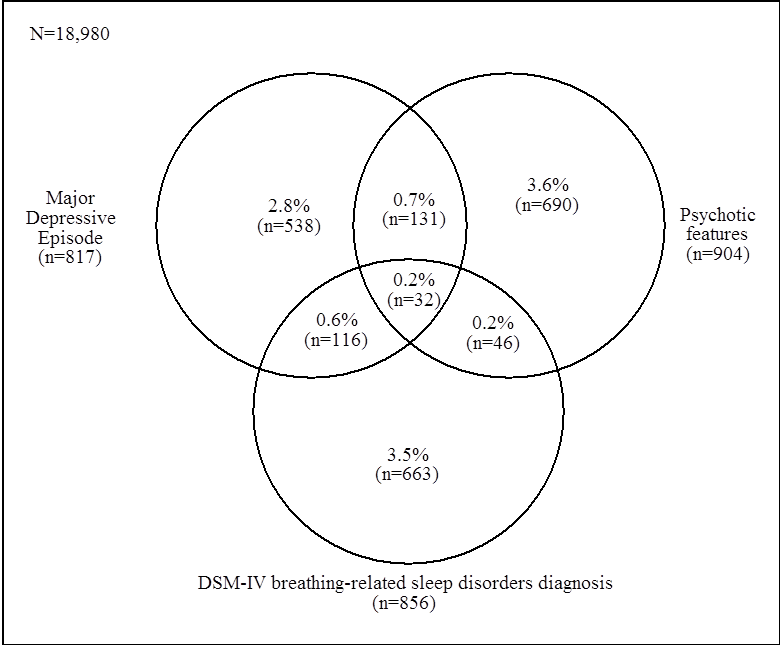
Time sequence analyses from recent studies (Ohayon and Roth 2003; Johnson et al., 2006) show that the onset of insomnia precedes the onset of depression in most of the cases (Figure 1). These results would suggest a directional pattern of development from insomnia to depression independently of age.
Is this association between insomnia and depression translated into sleep abnormalities? Important changes in the sleep architecture of depressed patients have been documented since for over than 30 years. Decreased sleep efficiency, reduction of slow-wave sleep, reduced REM sleep latency and prolonged first REM period are among the most prominent traits of sleep abnormalities in depression. These architectural sleep changes are not specific to depression and have been observed in other psychiatric disorders. They have therefore no diagnostic relevance in identifying patients with depression. Interestingly, follow-up studies have revealed that the normalization of the sleep architecture was associated with a lower risk of relapse into depression while persistence of decreased REM sleep latency increased risks of relapse. Sleep-endocrine studies in primary chronic Insomnia and depression show similarities in their results; with an increase in the ACTH and cortisol secretion throughout the night or the 24-hour period (Vgontzas et al., 2001; Antonijevic et al., 2000; Kunugi et al., 2006). Cortisol levels and ACTH decrease during recovery from depression suggesting that hypercortisolism is a state marker of depression in adults. No study has examined ACTH and cortisol secretion in remitted insomnia patients. It still unclear if specific symptom patterns in depression are more likely to be associated with abnormal ACTH and cortisol secretion. From existing studies, the proportion of depressive patients with abnormal ACTH and cortisol levels is unknown. Therefore, it could be possible that depressive patients with elevated cortisol levels have insomnia complaints. It could also explain why gender differences on cortisol levels have been observed in depressive patients; depressive women having elevated cortisol levels (Antonijevic et al., 2000). Women more frequently than men report insomnia, even within major depressive disorder. Consequently, the possibility that the increase in the ACTH and cortisol secretion is an effect of sleep disturbances cannot be discarded without more controlled clinical studies.
It exists numerous pharmacological and non-pharmacological treatments for depression. Among non-pharmacological treatment, sleep deprivation has been proven one of the most fast acting and efficient treatment. Improvement in depressive symptoms occurs after only a single night of total sleep deprivation in 50% to 60% of depressive patients. No other antidepressant treatment has these effects within 24 hours. Partial sleep deprivation regimens have also been tested and were found as effective as total sleep deprivation. To have lasting effects, partial or complete sleep deprivation has to be applied up to three times per week. However, beneficial effects of partial or total sleep deprivation disappear after one night of recovery sleep and are mitigated by naps and micro sleep during the day following sleep deprivation. Systematic investigations of endocrine changes following total or partial sleep deprivation are scant and no definite conclusions can be drawn.
In healthy young adults, total sleep deprivation was associated with a decrease in cortisol levels the next day and during the recovery night (Vgontzas et al., 1999). Decrease in cortisol levels and ACTH were also observed among unmedicated depressive patients after one night of total sleep deprivation (Murck et al., 2006). However, the mechanisms underlying mood improvement of depressed patients following sleep deprivation remain unknown.
