Severe Hot Flashes are associated with Chronic Insomnia and Global Sleep Dissatisfaction
First created | 02/04/2006
Last edited |
- Ohayon MM. Severe hot flashes are associated with chronic insomnia. Arch Intern Med. 2006;166:1262-1268.
Because hot flashes also occur during the night, their presence has been frequently associated with insomnia in women with symptoms of menopause. However, many factors other than hot flashes or menopause can be responsible for insomnia and several factors associated with insomnia in the general population are also commonly observed in perimenopausal and postmenopausal women with hot flashes.
It has been reported that insomnia complaints significantly increase with age in both men and women, but more importantly in women. The augmentation in the prevalence of insomnia in women coincides with the age when menopause begins (1).
Hot flashes are climacteric vasomotor symptoms that affect up to 85% of menopausal women (2-9). These symptoms frequently persist up to five years after the last menstrual cycle. They are also one of the first climacteric symptoms to appear in premenopausal women: Nearly 20% of premenopausal women in their late forties report hot flashes (7, 10, 11). Their severity increases in late perimenopause and postmenopause (11).
Because hot flashes also occur during the night, their presence have been frequently associated with sleep disturbances, mainly insomnia, in symptomatic menopausal women (2,7,12,13,14). However, many factors other than hot flashes or menopause can be responsible for insomnia complaints: several factors associated with insomnia in the general population are also commonly observed in peri- and postmenopausal women with hot flashes. This is the case, for example, with anxiety and depression that are frequent in both insomnia and menopause (15-17).
On the other hand, poor health status and sleep apnea, two other factors associated with insomnia complaints, increase with age, putting women that are in peri- and postmenopausal periods at greater risk for complaining of insomnia (18,19). Consequently, the lack of adequate controls for other factors associated with insomnia may influence its association with hot flashes.
This study, performed in the general population, aims:
- to assess the prevalence and severity of hot flashes in pre-, peri- and postmenopausal women aged between 35 and 65 years old and,
- to determine if hot flashes remain associated with insomnia complaints after controlling for variables commonly associated with insomnia.
METHODS
SAMPLE
The study was performed in 2003 and 2004. The target population was composed by the 24 million adults (18 years and older) living in the state of California (USA). A total of 3,243 subjects out of 3,787 eligible individuals participated in the survey (participation rate 85.6%).
PROCEDURES
In the first stage, telephone numbers were pulled out proportionally to the population size of each county in California.
In the second stage, during the telephone contact, the Kish method (20) was used to select one respondent per household.
This method allowed for the selection of a respondent based on age and gender to maintain a sample representative of these two parameters. If the household member chosen declined to participate, the household was dropped and recorded as refusal and the process repeated.
Interviewers explained the goals of the study to potential participants. They requested verbal consent before conducting the interview. The participants had the option of calling the principal investigator if they wanted further information. The study was reviewed by the Stanford University Institutional Review Boards (IRB).
Subjects who declined to participate or who gave up before completing half the interview were classified as refusals even though they might have met an exclusion criterion. Excluded from the study were subjects who were not fluent in English, who suffered from a hearing or speech impairment or with an illness that precluded being interviewed.
Phone numbers were dropped and replaced only after a minimum of 10 unsuccessful dial attempts were made at different times and on different days, including weekdays and weekends.
An added-digit technique, that is, increasing the last digit of a number by one, was employed to control for unlisted telephone numbers. The final sample included 21.4% unlisted telephone numbers.
The interviews lasted on average 74.5 (+-37.8) minutes. An interview could be completed with more than one telephone call when it exceeded 60 minutes or at the request of the participant.
The project manager or the team leaders also called nearly all the participants who completed the interview. During this 6-8 minutes call, they asked a series of random questions related to the interview and also asked the participants how satisfied they were with the interviewer.
INSTRUMENT
Interviewers used the Sleep-EVAL knowledge-based expert system (21,22) to conduct the interviews. This computer software is specially designed to administer questionnaires and conduct epidemiological studies in the general population. In Sleep-EVAL, the reasoning process is performed by a non-monotonic, level-2 inference engine. This engine uses the resources of two neural networks, a mathematical processor, the knowledge base and the base of facts. The interview begins with a questionnaire asked to all the participants. It includes, in order of appearance:
- sociodemographic information
- sleep/wake schedule
- sleeping habits
- sleep disturbance symptoms
- medical and paramedical consultations in the last 12-month period
- hospitalizations in the last 12-month period
- physical diseases
- use of prescribed drugs
- use of non-prescribed drugs
- health quality assessment scale
- alimentation scale
- fatigue scale
- pain questionnaire
- height and weight
- for women only, a questionnaire on menopause
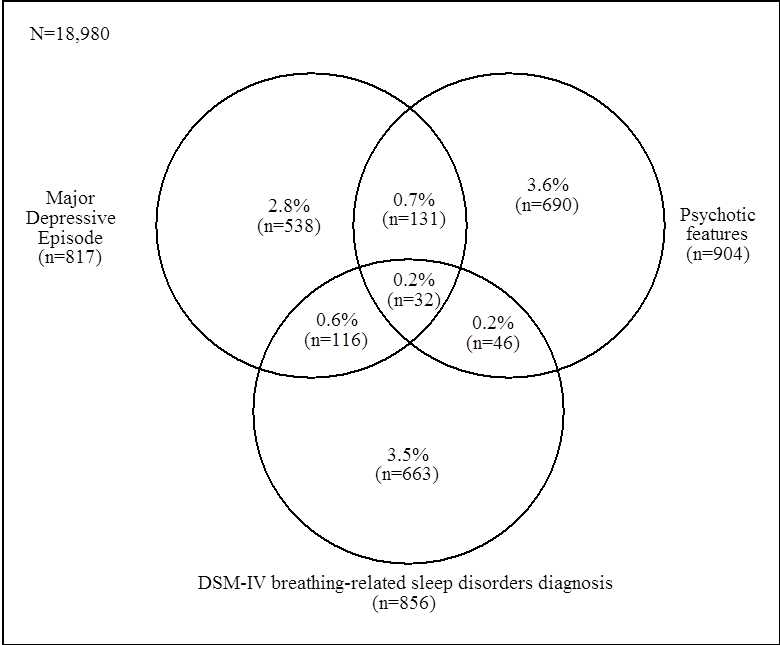
Once this information is collected, the system begins the diagnostic exploration of sleep and mental disorders. On the basis of responses provided by a subject to this questionnaire, the system formulates an initial diagnostic hypotheses that it attempts to confirm or reject by asking supplemental questions or by deductions. Concurrent diagnoses are allowed in accordance with the DSM-IV (23) and the International Classification of Classification of Sleep Disorders (24). The system terminates the interview once all diagnostic possibilities are exhausted.
The differential process is based on a series of key rules allowing or prohibiting the co-occurrence of two diagnoses.
The questionnaire of the expert system is designed such that the decision about the presence of a symptom is based upon the interviewee's responses rather than on the interviewer's judgment.
The system has been tested in various contexts in clinical psychiatry and sleep disorders clinics (25-28). In psychiatry, kappas have ranged from 0.44 (schizophrenia disorders) to 0.78 (major depressive disorder) (25,26). In sleep medicine, kappas have ranged from 0.68 to 0.92 (27,28).
DEFINITIONS
1) Menopausal status was classified in accordance with the World Health Organization definition (29):
- Premenopause: Women aged 35 years or older who reported having regular menstrual cycles in the last year.
- Perimenopause: Women who reported irregular menstrual cycles in the last year and had at least one menstrual bleed in the previous year.
- Postmenopause: Women who reported no menstrual bleed in the last 12-month period.
2) Hot flashes had to occur at least three days per week. Last month severity of hot flashes was defined as follows:
- Mild: Most of the time hot flashes are limited to a sensation of heat without sweating;
- Moderate: Most of the time hot flashes are a sensation of heat with sweating but not enough to prevent the pursuit of activity;
- Severe: Most of the time hot flashes are a sensation of heat with sweating causing the woman to stop her activity.
3) Symptoms of insomnia were defined as:
- Difficulty Initiating Sleep (DIS),
- Difficulty Maintaining Sleep (DMS),
- Non-Restorative Sleep (NRS).
- Global Sleep Dissatisfaction (GSD) was defined as a complaint about sleep quality or quantity.
It was required for all these symptoms to be present at the time of the interview at least 3 nights per week for at least the past 6 months.
4) Chronic insomnia diagnosis was defined according to DSM-IV classification with the exception that insomnia duration was set at 6 months instead of 1 month.
OTHER VARIABLES ASSESSED
The following variables were also collected:
- Sociodemographic variables: age, gender, marital status, ethnic origin, occupation and income.
- Health status variables: subjective assessment of health quality (from very poor to excellent); physical diseases at the time of the interview; chronic pain (lasting at least 6 months); blood pressure; medications (prescribed or not, including hormono replacement therapy); medical consultations in the previous year.
- Height and weight in order to calculate the Body Mass Index (BMI). The BMI categories were defined as recommended by the National Heart, Lung and Blood Institute (30). Subjects were: a) underweight: BMI lower than 18.5 kg/m2; b) normal: BMI between 18.5 and 25 kg/m2; c) overweight: BMI between 25 and 29.9 kg/m2; d) obese: BMI >= 30 kg/m2.
- Breathing pauses during sleep lasting some seconds were coded present when the subject reported a frequency of at least 3 nights per week.
ANALYSES
Bivariate analyses were performed using the chi-square test or the Fisher's exact test when n values were smaller than 5. Logistic regressions were used to compute the odds ratios (OR) associated with insomnia complaints. Reported differences were significant at the .05 level or less.
RESULTS
The sample was composed of 3,243 subjects aged between 18 and 94 years. It included 982 women aged from 35 to 65 years. Of these women, 57.2% (n=562) were in premenopause; 22.3% (n=219) in menopause and 20.5% in postmenopause (n=201).
Demographic characteristics of these three groups are presented in Table 1.
As seen, premenopausal women were younger and more likely to be working than the two other groups. Postmenopausal women were more likely to be overweight than the two other groups.
Menopause:
- had begun at the age of 40 years or earlier in 13.6% of cases;
- in 9.3% it began between 41 and 44 years old;
- in 12.2% at 45 or 46 years; 16.5% at 47 or 48 years;
- 25.5% at 49 or 50 years;
- 10% at 51 or 52 years;
- and in 11.9% at 53 years or older.
The average age at natural menopause was 50.3 (+-3.0) years. Hormone replacement therapy was taken by:
- 20.8% of perimenopausal women and
- 13.2% of postmenopausal women.
PREVALENCE OF HOT FLASHES
A total of 32.8% of the women reported having hot flashes:
- the prevalence was 12.5% in the group of premenopausal women;
- it rose to 79.0% in the perimenopausal group;
- it decreased to 39.3% in the postmenopausal group (p<.0001).
Figure 1 details this prevalence according to the severity of hot flashes:
- about half of the women experienced mild hot flashes;
- nearly a third experienced moderate hot flashes
- and 15.5% experienced severe hot flashes.
Half of the women (50.9%) also experienced night sweats (in addition of daytime hot flashes).
PREVALENCE OF CHRONIC INSOMNIA SYMPTOMS
The presence of chronic insomnia was examined in association with the severity of hot flashes and the menopausal status.
As can be seen in Table 2, chronic insomnia dramatically increased among women with severe hot flashes. More than 80% (81.3%) of women with severe hot flashes had chronic insomnia symptoms.
Difficulty initiating sleep, non-restorative sleep, and global sleep dissatisfaction significantly increased in women with severe hot flashes but were comparable between women with mild hot flashes and those without hot flashes. Chronic difficulty maintaining sleep constantly increased with the severity of hot flashes.
When insomnia was examined in relationship to the menopausal status, chronic difficulty initiating sleep, chronic non-restorative sleep and global sleep dissatisfaction were more frequent among perimenopausal women. Difficulty maintaining sleep was lower among premenopausal women. A third (31.8%) of perimenopausal and postmenopausal women also reported that, in their opinion, insomnia was related to the development of menopause.
As seen in figure 2, perimenopausal women with hot flashes were more likely to link insomnia with menopause than were women without hot flashes. This association was not observed, however, in postmenopausal women.
Figure 2. Association between severity of hot flashes and insomnia (C
When examining the temporal relationship between insomnia and hot flashes, it was found that insomnia pre-dated menopause in 53.1% of perimenopausal women who reported insomnia symptoms and 21.4% of postmenopausal women (p<.0001) (Figure 3).

MULTIVARIATE MODELS
Several factors are likely to affect the bivariate associations observed between insomnia, hot flashes and menopausal status. Therefore, logistic regression analyses were performed to account for other variables that may have independent effects on sleep disturbances. Chronic insomnia symptoms were entered as dependent variables. More specifically, five models were calculated:
- chronic difficulty initiating sleep;
- chronic difficulty maintaining sleep;
- chronic non-restorative sleep;
- at least one chronic insomnia symptom; and
- global sleep dissatisfaction.
The choice of independent variables was made in conjunction with their positive association with insomnia complaints in bivariate analyses.
The models included:
- marital status,
- occupation,
- race,
- severity of hot flashes,
- menopausal status,
- perceived health quality,
- Body Mass Index,
- hypertension,
- physical disease,
- chronic pain,
- major depressive disorder and
- anxiety disorders,
- level of stress,
- smoking,
- alcohol and coffee intake,
- breathing pauses during sleep,
- restless legs syndrome and
- periodic limb movement symptoms.
Age was not entered because of its strong correlation with menopausal status. The results are presented in table 3.
As it can be seen, the likelihood of having chronic difficulty initiating sleep, chronic non-restorative sleep or at least one chronic insomnia symptom increased with the severity of hot flashes. On the other hand, menopausal status was significant only for chronic difficulty maintaining sleep; postmenopausal women had a higher likelihood of reporting chronic difficulty maintaining sleep.
Other variables significantly associated with insomnia were:
- one's health perception as being poor,
- breathing pauses during sleep, and
- chronic pain (chronic difficulty maintaining sleep; chronic non-restorative sleep and chronic insomnia).
Major depressive disorder was significant only in the model where "at least one chronic insomnia symptom" was the dependent variable (Table 3). Similarly, Caucasian ethnicity was significant only for difficulty maintaining sleep (OR:1.5 (1.0-2.1); p=.05).
Marital status, occupation, Body Mass Index, anxiety disorders, level of stress, smoking, alcohol, coffee intake restless legs syndrome and periodic limb movement symptoms were non-significant for all four insomnia symptom models.
The fifth model, global sleep dissatisfaction, gave similar results for the severity of hot flashes, one's health perception as poor, chronic pain and breathing pauses during sleep. Pre- and perimenopausal women had higher likelihood of reporting global sleep dissatisfaction. Additionally, high level of stress (OR: 1.7 (1.1-2.9); p<.01), drinking at least 3 cups of coffee per day (OR 1.6 (1.0-2.6); p=.05) and restless legs syndrome (OR: 1.8 (1.1-3.2); p<.05) were associated with global sleep dissatisfaction.
A sixth model with insomnia diagnosis as the dependent variable, revealed that were associated with the presence of an insomnia diagnosis:
- one's health perception as hot flashes:
- poor (OR: 3.0 (1.5-5.8); p=.001);
- mild (OR: 2.2 (1.1-4.3); p=.02);
- moderate (OR: 3.5 (1.8-7.1); p<.001);
- severe (OR: 2.5 (1.0-5.9); p=.05);
- chronic pain (OR: 2.3 (1.4-3.8); p=.002);
- and being Caucasian (OR: 2.0 (1.1-3.6); p=.02).
DISCUSSION
This study provides evidence that severe hot flashes are associated with chronic insomnia complaints in women aged between 35 and 65 years.
Generally speaking, severe hot flashes increased the likelihood of reporting global sleep dissatisfaction , chronic difficulty initiating sleep and chronic non-restorative sleep. Menopausal status, on the other hand, was associated with insomnia complaints only for chronic difficulty maintaining sleep and global sleep dissatisfaction. The multiplicity of factors associated with insomnia complaints illustrates the multi-factorial aspects of chronic insomnia in women.
Compared to previous epidemiologic studies conducted in midlife women, this study is unique in several aspects:
- First, the severity of hot flashes was studied. The dramatic increase in insomnia complaints in women with severe hot flashes indicates that severity of hot flashes should be routinely assessed in all studies on menopause.
- Second, insomnia symptoms were defined in terms of frequency and chronicity. This strict definition permitted us to limit the evaluation to the most enduring insomnia symptoms and not transitory phenomena.
- Third, the variables assessed covered a broad range of potential factors associated with insomnia. Most epidemiologic studies had used a limited set of confounding variables to evaluate the association between hot flashes and/or menopausal status and insomnia.
The prevalence of hot flashes observed in menopausal women in that study is comparable to that reported in other epidemiologic studies performed in the United States (2-5). Similar prevalence of hot flashes was also reported in Europe (6), Australia (7), and Asia (8,9). In this sample, the age at natural menopause was comparable to that reported in other American studies (31-33).
It was found that 56.6% of perimenopausal women and 50.7% of postmenopausal women had at least one chronic insomnia symptom. This is higher than the rate reported in studies that evaluated difficulty sleeping with a single yes/no question. For example, Kravitz et al (13) found that between 39.6% and 45.4% of peri- and postmenopausal American women reported difficulty sleeping in the two weeks prior to the interview. Another American study reported a rate of about 40% in peri- and postmenopausal women (2). An Australian study found rates between 44% and 52% in peri- and postmenopausal women (7) and a Chinese study found a rate of about 21% of trouble sleeping in pre, peri- and postmenopausal women (14). Results showed that chronic insomnia considerably increased in peri- and postmenopause compared to premenopause: More than half of the women reported difficulty initiating or maintaining sleep or non-restorative sleep.
Several studies have attributed the increase in sleep disturbances to hot flashes in the perimenopausal period (34,35). However, this may be too simplistic, since many other factors such as chronic pain and poor health also increased with age. Both of these factors are closely related to insomnia complaints.
Their importance is illustrated in the multivariate models: The association between chronic insomnia and menopausal status considerably diminished and even disappeared for difficulty initiating sleep and nonrestorative sleep while chronic pain and poor health remained significant. It should be noted that postmenopausal women still had a higher probability of reporting difficulty maintaining sleep. A possible explanation is that since postmenopausal women are older than the two other groups of women, this association is mostly due to aging rather than menopausal status.
Other sleep disorders, such as periodic limb movements, restless legs syndrome and obstructive sleep apnea, are known to increase with age and to be associated with insomnia complaints. Periodic limb movements and restless legs syndrome did not reach significant levels in our multivariate models. However, their inclusion decreased the odds between hot flashes and insomnia.
Objective polysomnographic measures of sleep disturbances in menopausal women have given conflicting results. Some studies have demonstrated a significant correlation between the occurrence of hot flashes and waking during sleep (36-38) while others found no evidence that hot flashes disturb sleep in healthy women (39-41). Several factors for the lack of association may have influenced the results. Most of these polysomnographic studies are based on small samples. Therefore, it was difficult to examine the data using different factors such as the severity of hot flashes or the report of frequent nocturnal awakenings.
As our results illustrated, about 55% of women with hot flashes complained of difficulty maintaining sleep and the number of women with insomnia complaints increased with severe hot flashes. Furthermore, the complaint may not be difficulty maintaining sleep but other insomnia symptoms such as non-restorative sleep. Indeed, it is likely that hot flashes occurring during the night have different levels of severity and cause more or less discomfort leading to different complaints or no complaint at all.
It should be kept in mind that this is a cross-sectional study. Therefore, it presents a picture of the population at a given point in time: For example, it was possible to identify the association between the severity of hot flashes and chronic insomnia but the ability to determine if causality existed was limited. Another limitation is that data are based on self-reports. Measurement of hot flashes relied on individual perception and experience. Moreover, studies that compared subjective and objective measurement of hot flashes found that women reliably described their hot flashes (42,43).
CONCLUSIONS
The results of this cross-sectional study indicate that insomnia in pre-, peri- and postmenopausal women are influenced by several factors such as chronic pain, poor health and sleep apnea, which are not related specifically to menopausal status but to aging.
On the other hand, hot flashes remain an important factor to explain the insomnia in midlife women independently of their menopausal status. Treating hot flashes can be a solution to improve the sleep quality and minimize deleterious consequences of chronic insomnia. Specific care must be taken with these midlife women to avoid unnecessary treatments and chronic sleep problems.