Sleep Apnea and Depression
First created | 05/04/2005
Last edited |
- Ohayon MM. The Effects of Breathing-Related Sleep Disorders on Mood Disturbances in the General Population. Journal of Clinical Psychiatry 2003; 64:1195-1200.
Breathing-related sleep disorders, such as obstructive sleep apnea syndrome and upper airway resistance syndrome, are disabling sleep disorders that may have important consequences on the daily functioning of affected individuals. These disorders are often accompanied by excessive daytime sleepiness and sometimes with cognitive impairments (1,2).
Symptoms of breathing-related sleep disorders are similar to neurovegetative features of depression. Some clinical studies have attempted to determine whether depression limits the recognition and treatment of breathing-related sleep disorders, or if breathing-related sleep disorders play a role in the etiology or course of depressive disorder.
To date, the results of these clinical studies have been mixed. Some have found that obstructive sleep apnea syndrome is associated with higher rates of clinical depression (2, 3, 4) or higher rates of depressive symptomatology (5, 6). Other clinical studies have found that obstructive sleep apnea patients do not have higher rates of depression than do individuals with other chronic diseases (7) or control subjects (8, 9). Some studies have also measured whether depressive symptomatology is lessened when a breathing-related sleep disorder is treated with continuous positive airway pressure (CPAP) (6, 10). However, the amelioration in the depressive mood could be due to a placebo effect of the CPAP (10).
One study that examined the sleep architecture of depressive patients with obstructive sleep apnea syndrome found that sleep latency was longer and the percentage of REM shorter in depressed patients without obstructive sleep apnea compared to depressed patients with obstructive sleep apnea (11). Obstructive sleep apnea is known to affect about 2% of the population (12,13). It is more frequent in men and increases with age.
Major depressive disorders have a prevalence of approximately 4% in the general population and it affects more frequently women than men (14,15). Data about breathing-related sleep disorders and depressive illness are documented only to a clinical level. The importance of this association in the general population remains undocumented.
METHODS
SAMPLING
The participants in five countries were interviewed by telephone between 1994 and 1999. The studied countries were:
- the United Kingdom,
- Germany,
- Italy,
- Portugal and
- Spain.
Ethical and research committees at the Imperial College (London, UK), the Regensburg University (Germany), the San Raffaele Hospital (Milan, Italy), the Santa-Maria Hospital (Lisbon, Portugal) and the Hospital General Univ. Vall d'Hebron (Barcelona, Spain) approved the study. The target population was all non-institutionalized residents aged 15 years or over with the exception of Portugal, where the minimum age was set at 18 years at the recommendation of the Portuguese ethics committee. This represented about 206 million Europeans. A two-stage design was used for all countries:
- The population of each country was first divided according to its geographical distribution as per the official census data, then telephone numbers were randomly drawn in each geographical area.
- Second, within each household, a member was selected by age and gender using the Kish method (16) in order to maintain the representation of the sample and to avoid bias related to non-coverage error.
Participants had to first grant their verbal consent prior to proceeding with the interview. For subjects younger than 18 years of age, the verbal consent of the parent(s) was also requested. We excluded potential participants who had insufficient fluency in the national language, who had a hearing or speech impairment or with an illness that precluded the feasibility of an interview.
The participation rate was:
- 79.6% (4,972 of 6,249 eligible individuals) in the UK;
- 68.1% (4,115 of 6,047 eligible individuals) in Germany;
- 89.4% (3,970 of 4,442 eligible individuals) in Italy;
- 83% (1,858 of 2,234 eligible subjects) in Portugal; and
- 87.5% (4,065 of 4,648 eligible individuals) in Spain.
A total of 18,980 subjects participated in the study. The overall participation rate was 80.4%.
INSTRUMENT
The Sleep-EVAL expert system (17,18), a software specifically designed to conduct epidemiological studies in the general population and to administer questionnaires, was used to perform the interviews.
Lay interviewers read to the subjects the questions displayed on the computer screen and entered the answers in the Sleep-EVAL system. The knowledge base of the Sleep-EVAL system comprised a standard questionnaire and diagnostic pathways covering the International Classification of Sleep Disorders (ICSD) (19) and the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) (20).
The questionnaire consisted of sociodemographic information, sleep/wake schedule, physical health queries and questions related to sleep and mental disease symptoms. Interviews typically began with general questions about demographic characteristics, followed by questions about sleeping habits. The interviews progressed to more private questions regarding mental health.
The system used the answers to select a series of plausible diagnostic hypotheses (causal reasoning process). Further questioning and deductions of the consequences of each answer allowed the system to confirm or reject these hypotheses (non-monotonic, level-2 feature). The differential diagnosis process was based on a series of key rules allowing or prohibiting the co-occurrence of two diagnoses in accordance with ICSD and DSM-IV prescriptions. The interview ended once all diagnostic possibilities were exhausted.
The system has been tested in various contexts; in clinical psychiatry, overall kappas between the diagnoses of four psychiatrists and those of the system ranged from .44 with one psychiatrist to .78 with two psychiatrists (n=114 cases) (21). Another study involved 91 forensic patients. Most of the patients (60%) received a diagnosis in the psychosis spectrum. The kappa between diagnoses obtained by the system and those given by psychiatrists was .44 for specific psychotic disorders (mainly schizophrenia) (22).
In a study performed in the general population (n=150), the diagnoses obtained by two lay interviewers (inexperienced in sleep and psychiatric assessments) using Sleep-EVAL were compared to those obtained by two clinician psychologists. A kappa of .85 was obtained in the recognition of sleep problems and of .70 for insomnia disorders.
Validation studies performed in sleep disorders clinics (Stanford University, Regensburg University and Toronto Hospital) testing the diagnoses of the system against those of sleep specialists using polysomnographic data gave kappas of .93 and .92 with the diagnosis of obstructive sleep apnea syndrome, and kappas of .78 and .71 with insomnia (23,24).
The duration of the interviews ranged from 10 to 333 minutes with an average of 40 minutes (+-20 minutes). The longest interviews involved subjects with multiple sleep and mental disorders. Interviews were completed over two or more sessions if the duration exceeded 60 minutes.
DEFINITIONS
DSM-IV breathing-related sleep disorder: It includes subjects who complained of a disrupted sleep associated with excessive daytime sleepiness or insomnia due to abnormalities and ventilation during sleep.
This included:
- subjects with obstructive sleep apnea syndrome (breathing pauses during sleep at least three nights per week accompanied by insomnia or excessive daytime sleepiness), and
- subjects who reported choking, being airless or with a loud snoring interrupted by pauses or choking during sleep at least three nights per week accompanied by excessive daytime sleepiness, disrupted sleep or non-restorative sleep.
This corresponded to the DSM-IV description of breathing-related sleep disorder.
DSM-IV major depressive episode: It includes subjects who meet all the criteria of a major depressive episode with the exception of the criterion B (mixed depressive - manic episodes).
Psychotic features: Subjects answered a series of questions about delusions and hallucinations (25,26). Each question was answered on a frequency scale (never; less than once a month; 1 to 3 times a month; 1 time a week; 2 to 5 times a week; 6 to 7 times a week). Delusions and/or hallucinations associated with depressive mood occurred at least 6 to 7 times a week in order to cast off subjects who may have transient phenomena.
ANALYSES
A weighting procedure was applied to correct for disparities in the geographical, age and gender distribution between the sample and each studied country. This procedure was to compensate for any potential bias from such factors as an uneven response rate across demographic groups. Results were based on weighted n values. Percentages for target variables were given with 95% confidence intervals (95% C.I.).
Bivariate analyses were performed using the chi-square test.
Each class of variables was analyzed using logistic regressions (27). Ninety-five percent confidence intervals were calculated for prevalence rates and odds ratios. Reported differences were significant at .05 or less.
RESULTS
PREVALENCE OF BREATHING DISORDERS
In this sample, the prevalence of obstructive sleep apnea syndrome was 2.1%. The prevalence was higher in men (2.6%) than in women (1.6%) and increased with age (Table 1).
The prevalence of any other type of breathing-related sleep disorders diagnosis was 2.5%. The rates were comparable between men and women but it significantly increased with age for men and women (Table 1).
Therefore, the total prevalence of breathing-related sleep disorders was 4.6% in the sample.
PREVALENCE OF MAJOR DEPRESSIVE EPISODE
The prevalence of major depressive episode as defined above was 4.3% in the sample. The prevalence was significantly higher in women (5.3%) than in men (3.2%) and was significantly lower in the oldest age group compared with younger age groups (Table 1).
PREVALENCE OF PSYCHOTIC FEATURES
Overall, 4.8% of the sample reported hallucinatory or delusional experiences at least several days per week. The prevalence was higher in women (5.4%) than in men (4.1%) and higher in youngest subjects (Table 1).
ASSOCIATION BETWEEN BREATHING-RELATED SLEEP DISORDERS, MAJOR DEPRESSIVE EPISODE AND PSYCHOTIC FEATURES
Figure 1 presents the associations among the three variables. 
As can be seen, the association between Major Depressive Episode and a DSM-IV breathing-related sleep disorders diagnosis was present in 0.8% of the whole sample.
The association between major depressive episode and psychotic features was observed in 0.9% of the sample and the association between DSM-IV breathing-related sleep disorders diagnosis and psychotic features was in 0.4% of the sample. The triple association (Major Depressive Episode, DSM-IV breathing-related sleep disorders diagnosis and psychotic features) was found in 0.2% of the sample.
In figure 2, it can be seen that the prevalence of DSM-IV breathing-related sleep disorders diagnosis is the highest among subjects with a major depressive episode:
- 19.6% of depressive subjects with psychotic features and
- 17.7% of depressive subjects without psychotic features have a DSM-IV breathing-related sleep disorders diagnosis.
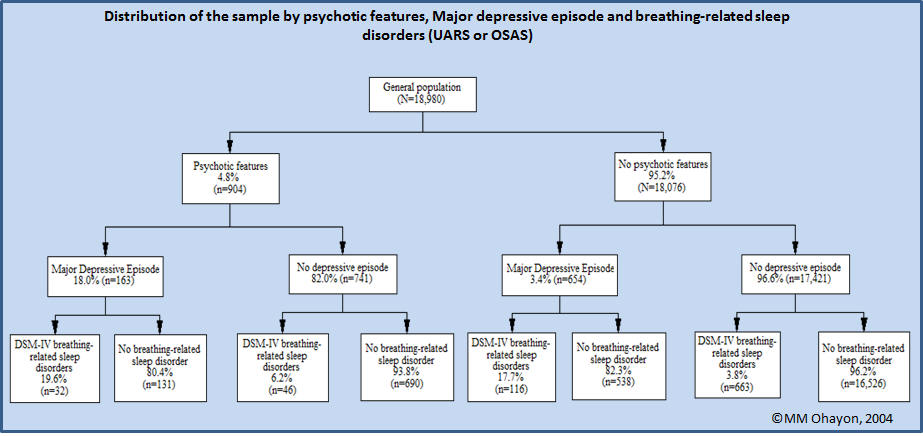
The risk of having a DSM-IV breathing-related sleep disorders diagnosis is 5.33 (95% C.I.: 4.40-6.48) higher in depressed subjects compared with non-depressed subjects.
The prevalence of a DSM-IV breathing-related sleep disorders diagnosis is also higher among non-depressed subjects with psychotic features (6.2%) compared to non-psychotic and non-depressed subjects (3.8%).
ROLE OF CONFOUNDING VARIABLES IN THE ASSOCIATION MAJOR DEPRESSIVE EPISODE AND BREATHING-RELATED SLEEP DISORDERS
Several factors can explain the association between major depressive episodes and breathing-related sleep disorders. It is well-known that obesity, hypertension, age and gender are important factors in both major depressive disorders and breathing-related sleep disorders. A logistic regression was calculated to control for such factors.
The results of Table 2 show that Major Depressive Episode and the presence of psychotic features remain strongly associated to the presence of a DSM-IV breathing-related sleep disorders diagnosis even when other important factors (obesity and hypertension) for a DSM-IV breathing-related sleep disorders diagnosis are taken into account. Subjects with a major depressive episode are five times more likely to have a DSM-IV breathing-related sleep disorders diagnosis than non-depressed individuals.
The introduction of the interaction Major Depressive Episode and psychotic features into the model does not change the results: Major Depressive Episode with or without psychotic features remains strongly associated with a DSM-IV breathing-related sleep disorders diagnosis. This was also the case for psychotic features alone. Use of antidepressants or neuroleptics were not significantly associated with a DSM-IV breathing-related sleep disorders diagnosis in this multivariate model.
DISCUSSION
To our knowledge, this is the first time that an epidemiological study has attempted to estimate the association between breathing-related sleep disorders and major depressive disorders. Our results show that 0.8% of the general population have both disorders; this represents about 800 individuals out of 100,000.
COMPARISON OF PREVALENCES WITH OTHER COMMUNITY-BASED STUDIES
Obstructive sleep apnea syndrome (OSAS): Existing prevalence rates for OSAS have been mainly derived from studies on cohorts or from selected samples (13, 28, 29) rather than from representative samples of the general population.
The prevalence of OSAS observed in this sample is similar to the rate reported by Young et al. (13) in the Wisconsin cohort when comparing the same age range. Major depressive disorders: In this study, the point prevalence of a DSM-IV major depressive episode (4.3%) is comparable to the one-month prevalence reported in the National Comorbidity Survey (NCS) (4.9%) (15) but it is higher than the prevalence obtained in the Epidemiological Catchment Area (ECA) survey (2.2%) (14).
The main difference is in the definition of major depressive episode. In this study, to include as many individuals as possible who had a major depressive episode, we did not exclude individuals who also fulfilled the criteria for a manic episode (like the NCS study). When we excluded the individuals with substance abuse or dependence, bipolar disorders or non-affective psychosis, the prevalence of a major depressive episode dropped to 2.4%, which is close to the ECA rate and close also to the 2.1% rate of "pure episode" of major depression reported in the NCS study.
ASSOCIATION BETWEEN BREATHING-RELATED SLEEP DISORDERS AND MAJOR DEPRESSIVE DISORDERS
We found a high positive association between major depressive disorder and breathing-related sleep disorders, depressive subjects being five times more likely to have breathing-related sleep disorders than non-depressed subjects.
This association remains strong and positive even when controlling for other important factors such as obesity and hypertension. This result is different from a clinical study that found the association between a breathing-related sleep disorder and depressive symptoms disappeared when controlling for BMI and hypertension (30). This can be due to the fact that these authors measured only sleep apnea (respiratory disturbance index >=15 events per hours) and based the presence of depression on the CES-D scale.
The contradiction found in the literature about the association between breathing-related sleep disorders and depression can be related to the definition used. Some studies used only the respiratory disturbance index as a measure of the presence of a breathing-related sleep disorder. However, obstructive sleep apnea syndrome and breathing-related sleep disorders diagnosis are more complex clinical entities that require the presence of other clinical symptoms such as excessive daytime sleepiness or non-restorative sleep, two symptoms that are often observed in depressed patients. Other studies have attempted to relate the severity of the breathing-related sleep disorder using the RDI to the presence of depression (31). The severity of the RDI did not appear related to the presence of depression. However, the severity of clinical symptoms of breathing-related sleep disorders was not assessed. The severity of fatigue or daytime sleepiness associated with the breathing-related sleep disorder may have influenced the presence of a depressive disorder.
We also found that psychotic features were positively associated with breathing-related sleep disorders but not as strongly as major depressive episodes. The association remained even when controlling for the presence of major depressive episodes. These associations have been seldom investigated although some cases have been reported (32,33).
In conclusion, nearly one fifth of subjects with a breathing-related sleep disorder also have a major depressive disorder and a similar proportion of individuals with depressive disorder have a breathing-related sleep disorder. The identification of one of these disorders should prompt physicians to investigate for the presence of the other disorder.
REFERENCE
Ohayon MM. The Effects of Breathing-Related Sleep Disorders on Mood Disturbances in the General Population. Journal of Clinical Psychiatry 2003; 64:1195-1200.
