Dyssomnia: Impact on Medical Diseases and Morbidity
First created | 12/01/2011
Last edited |
- Ohayon MM Dyssomnia: their Impact on Medical Diseases and Morbidity. SleepEval.com Website, 2010.
Dyssomnias are sleep disorders characterized by abnormalities in the quantity, quality or timing of sleep. The DSM-IV includes a chapter devoted to the sleep disorders. The chapter covers dyssomnias (characterized by abnormalities in the amount, quality or timing of sleep) and parasomnias (sleep disorders characterized by abnormal behavioral or physiological events occurring during sleep or during sleep-wake transitions).
Although insomnia complaints are reported by nearly one third of the general population, the diagnosis of insomnia is only made in 6-15%. Similarly, excessive daytime sleepiness is reported by approximately one in five people but only 2% of the general population are diagnosed with hypersomnia, narcolepsy, or behaviorally induced insufficient sleep syndrome. In the vast majority of individuals, sleep disturbances are caused by or associated with various medical or neurological diseases, psychiatric disorders, or environmental factors. Therefore, it is imperative to diagnose these comorbid conditions prior to planning appropriate treatment.
Sleep disturbances encompass a broad range of phenomena, such as insomnia, hypersomnia, sleep apnea, and restless legs syndrome (RLS). The latest edition of the International Classification of Sleep Disorders describes criteria for the diagnosis of >100 sleep disorders, divided into eight categories [1]:
- Insomnias
- Sleep related breathing disorders
- Hypersomnias of central origin
- Circadian rhythm sleep disorders
- Parasomnias
- Isolated symptoms, apparently normal variants, and unresolved issues
- Other sleep disorders
Most sleep disorders are accompanied by either insomnia, complaints of excessive daytime sleepiness (EDS), or both.
INSOMNIA
Insomnia symptoms are present in approximately 30% of the general population.
However, insomnia is diagnosed in only 6% [2].
Therefore, it can be estimated that approximately 75 million people in the US and 150 million in Europe are affected by insomnia.
Insomnia is usually chronic [3,4,5, 6,7], with most insomnia patients (85%) reporting that their symptoms have lasted ³1 year.
In fact, in one study, 68% of subjects reported their symptoms lasting ³5 years, while only 5% had symptoms that lasted 6-12 months, 6% 1-6 months, and just 4% had symptoms for ≤1 month [16].
WHAT MAY CAUSE INSOMNIA?
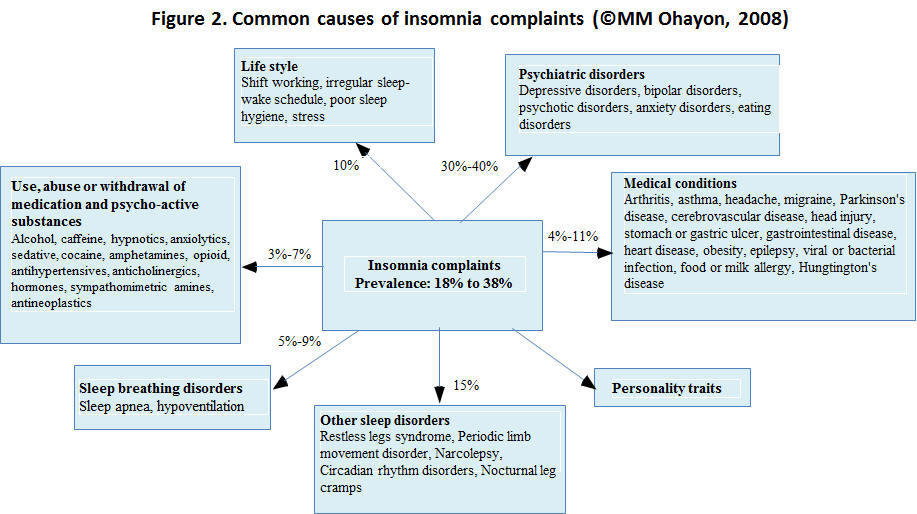
Insomnia has many different causes of insomnia and, according to the origin of the condition, insomnia may be divided into three main categories (Fig. 1):
- Comorbid with another physical and/or mental illness.
- Induced by use of psychoactive substances.
- Caused by lifestyle or without apparent cause.
Sleep-related breathing disorders (SRBD), such as obstructive sleep apnea syndrome (OSA) or hypoventilation, account for 5-9% of insomnia complaints (Fig. 2) [8-10].
Periodic limb movement disorders (PLMD), RLS, or both conditions are diagnosed in approximately 15% of individuals who present with insomnia complaints [9, 10, 11, 12].
Medical or neurological conditions are observed in 4-11% [4, 5, 9, 10].
Poor sleep hygiene or environmental factors are responsible for approximately 10% of insomnia complaints.
Finally, these symptoms are substance-induced in 3-7% [13,5, 9, 10].
MENTAL DISORDERS
Epidemiological studies have consistently reported that:
- mental disorders are associated with 30-40% of insomnia complaints.
- Symptoms of mental disorders are present in ³60% of individuals with insomnia symptoms [4,14-17].
MEDICAL CONDITIONS
In the general population, people with symptoms of insomnia have consistently been found to perceive their health to be poorer than the rest of the population [5,17-22] and ³50% do have recurrent, persistent, or multiple health problems [14,23].
The most frequently reported associations are with:
- upper airway diseases [5,24,25],
- rheumatic diseases [5,24,26,27], chronic pain [26,28], and
- cardiovascular diseases [5,29,30].
CONSEQUENCES OF INSOMNIA
DEVELOPMENT OF MEDICAL CONDITIONS
Several studies have attempted to determine whether insomnia can be responsible for cardiovascular accidents; however, the results have been inconclusive (Fig. 3).
One retrospective study found that insomnia was significantly predictive of myocardial infarction [31] and a prospective study reported that the relative risk (RR) of an individual with insomnia developing a cardiovascular accident was 3.1 [29].
Despite these results, three other prospective studies found no association between insomnia and the risk of developing a cardiovascular disease [32-34] while another found that there was a greater likelihood of developing insomnia after a cardiovascular accident [30]
DEVELOPMENT OF A MENTAL DISORDER
Four longitudinal studies have examined the relationship between the persistence of insomnia symptoms and the appearance of mental disorders [35-38]. They found that subjects with insomnia symptoms were 4-8 times more likely to develop a mental disorder during the year following the onset of these symptoms.
Two studies examining the time sequence of the appearance of insomnia symptoms in relation to that of mood and anxiety disorders reported that:
- insomnia was present in 70% of individuals with mood disorders and
- it preceded the appearance of the mood disorders in nearly 50% of cases.
Insomnia was found in one-third of patients with anxiety disorders and preceded the anxiety disorder in approximately 20% of cases [16,39].
REPERCUSSIONS FOR DAYTIME FUNCTIONING
Insomnia affects the daytime functioning of 20-60% of individuals with the disorder, [4, 8,40].
Individuals who sleep poorly ³3 nights per week, are dissatisfied with their sleep, do not feel rested upon awakening, and have hyperarousal in bed, are the most likely to experience repercussions in terms of their daytime functioning [4, 8].
ROAD, OCCUPATIONAL, AND DOMESTIC ACCIDENTS
In the general population, road accidents are experienced 2-3 times more frequently by drivers who are dissatisfied with their sleep, than those who report sleep satisfaction [8,18].
Such accidents are also more commonly experienced by those with short sleep times (defined as
<5 h less per night) [41,42].
In the elderly, insomnia is associated with an increased risk of hip fracture [43], and falls [44,45].
Furthermore, the RR for fatal occupational accidents in individuals who have difficulty in sleeping is 1.9 [46].
EXCESSIVE DAYTIME SLEEPINESS
Contrary to insomnia, EDS (defined as a propensity for sleep during waking hours) is not a diagnosis. EDS can be a symptom or a consequence of a sleep disorder, physical illness, or mental disorder. However, EDS is a disabling symptom that adversely affects various areas of quality of life and is a good indicator of the presence of health problems.
Excessive sleepiness is nearly as prevalent as insomnia, affecting approximately 20% of the general population [47].
WHAT MAY CAUSE EDS?
Like insomnia, EDS can be comorbid with several disorders such as organic diseases, mental disorders, and sleep disorders, or can be related to the abuse of or dependency on psychoactive substances. EDS can also be induced by the lifestyle of individuals or can be without apparent cause (Fig. 1).
In the general population:
- physical illnesses account for approximately 20% of EDS complaints,
- mental disorders for approximately 22%, and
- sleep disorders - such as OSA, RLS, and insomnia - for nearly 50%.
EDS is an essential criterion for the diagnosis of just three sleep disorders - behaviorally induced insufficient sleep syndrome, hypersomnia (idiopathic, recurrent, or post-traumatic), and narcolepsy. These conditions are diagnosed in >3% of the general population [65] (Fig. 4).
MENTAL DISORDERS
In epidemiological, cross-sectional studies, 12.4-30% of subjects with EDS have been shown to have a depressive disorder and 20-35% an anxiety disorder [48-51].
However, unlike insomnia, EDS has not been found to be associated with development of a mental disorder in longitudinal studies [35,36,52].
MEDICAL CONDITIONS
Several comorbid general medical and neurological disorders can cause EDS (Fig. 4).
Studies have shown that the risk of experiencing EDS is 2-4 times greater for people with diabetes than non-diabetics in the general population [51]. Other studies have observed that 16-74% of individuals with Parkinson's disease report EDS [53-55] and that elderly people who complain of EDS are three times more likely to have Alzheimer's disease [56].
In sleep clinics, OSAS is the most commonly seen cause of EDS, with ³75% of patients reporting EDS being diagnosed with OSAS. It has been shown that up to 25% of individuals in the general population who report EDS have OSAS [48-50, 57].
EDS AND LIFESTYLE
Unlike insomnia symptoms, EDS is generally not gender-related [49].
Whether its prevalence increases or decreases with age is not clear, as both trends have been observed [65].
Some work schedules, especially shift work, have frequently been often linked with EDS. Although some individuals may tolerate the physical strains caused by shift work, they are not immune to the fatigue, mood swings, reduced performance, and decreased mental agility caused by it. These problems are mainly due to the desynchronization of the circadian rhythm, that is, when the normal sleep/wake rhythm, the normal circadian rapid eye movement (REM) sleep rhythm, and the rhythm of REM and non-REM sleep patterns are disrupted. As a consequence, several shift workers complain of excessive sleepiness during working hours and of insomnia during sleeping time. Two studies have reported that up to 30% of night or shift workers report excessive sleepiness at work [46,18].
Epidemiological studies have reported higher risks of EDS in individuals who use antidepressants, anxiolytics, hypnotics, antihistamines, or alcohol (OR 2-6.7) [4,48,50].
EDS AND COGNITIVE DEFICITS
Two epidemiological studies have linked EDS to cognitive deficits.
In a study involving 2346 Japanese American men aged between 71 and 93 years, Foley et al. found that men who reported EDS at baseline were twice as likely to be diagnosed with dementia 3 years later than those who did not suffer from daytime sleepiness [58].
Ohayon and Vechierrini performed another study involving 1026 subjects aged ³60 years and controlled for age, gender, level of physical activity, occupation, organic diseases, use of sleep or anxiety medication, sleep duration, and psychological well-being [59]. They found that subjects with EDS were twice as likely to have attention-concentration deficits, difficulties in orientation, and memory problems than those without EDS.
EDS AND MORTALITY
Some population-based studies have investigated the mortality risks associated with EDS.
Hays et al. assessed mortality risk in a sample of 3962 elderly individuals (³65 years) and defined EDS by the presence of naps during the daytime [60]. They found that individuals who reported napping most of the time had a mortality risk of 1.73.
In another study by Rockwood et al., a small increased mortality risk (1.89) from daytime sleepiness was found in their elderly sample [61]. However, this risk did not retain significance when the model was adjusted for age, depression, cognitive deficits, and illness.
ROAD ACCIDENTS
EDS has been found to be a direct or contributing factor in 17-21% of road accidents [62,63]. Similarly, road accidents have been found to be experienced 2-3 times more frequently by drivers who have EDS [49,63].
CONCLUSION
Sleep disturbances are frequently associated with various medical or neurological conditions and psychiatric disorders.
Therefore, it is crucial to explore the possibility of comorbid conditions in patients who complain of sleep disturbances.
This should be the first step in the planning of an appropriate treatment strategy. Treatment of the comorbid condition may decrease sleep disturbances. However, in several instances, specific treatment of the sleep disturbances will be necessary and can contribute the management of the comorbid condition.
REFERENCES
- American Sleep Disorders Association Diagnostic Classification Steering Committee. International Classification of Sleep Disorders: Diagnostic and Coding Manual. Westchester, IL: American Academy of Sleep Medicine, 2005.
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 2002;6:97-111.
- Ohayon M. Epidemiological study on insomnia in the general population. Sleep 1996;19:S7-S15.
- Ohayon MM, Caulet M, Priest RG et al. DSM-IV and ICSD-90 Insomnia symptoms and sleep dissatisfaction. Br J Psychiatry 1997;171:382-8.
- Ohayon MM, Zulley J. Correlates of global sleep dissatisfaction in the German population. Sleep 2001;24:780-7.
- Ohayon MM, Partinen M. Insomnia and global sleep dissatisfaction in Finland. J Sleep Res 2002;11:339-46.
- Ohayon MM. Severe hot flashes are associated with chronic insomnia. Arch Intern Med 2006;166:1262-8.
- Ohayon MM, Roth T. What are the Contributing factors for insomnia in the general population? J Psychosom Res 2001;51:745-755.
- Buysse DJ, Reynolds CF 3rd, Hauri PJ et al. Diagnostic concordance for DSM-IV disorders: a report from the APA/NIMH DSM-IV field trial. Am J Psychiatry 1994; 151:1351-60.
- Jacobs EA, Reynolds CF 3rd, Kupfer DJ et al. The role of polysomnography in the differential diagnosis of chronic insomnia. Am J Psychiatry 1988;145:346-9.
- Edinger JD, Fins AI, Goeke JM et al. The empirical identification of insomnia subtypes: a cluster analytic approach. Sleep 1996;19:398-411.
- Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res 2002;53:547-54.
- Ohayon MM. Prevalence of DSM-IV diagnostic criteria of insomnia: Distinguishing between insomnia related to mental disorders from sleep disorders. J Psychiatr Res 1997;31:333-46.
- Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: prevalence and correlates. Arch Gen Psychiatry 1985; 42:225-32.
- Ohayon MM, Caulet M, Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatry 1998;39:185-97.
- Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res 2003;37:9-15.
- Maggi S, Langlois JA, Minicuci N et al. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. J Am Geriatr Soc 1998;46:161-8.
- Ohayon MM, Lemoine P, Arnaud-Briant V et al. Prevalence and consequences of sleep disorders in a shift worker population. J Psychosom Res 2002;53:577-83.
- Barbar SI, Enright PL, Boyle P et al. Sleep disturbances and their correlates in elderly Japanese American men residing in Hawaii. J Gerontol A Biol Sci Med Sci 2000;55:M406-11.
- Kim K, Uchiyama M, Okawa M et al. An epidemiological study of insomnia among the Japanese general population. Sleep 2000;23:41-7.
- Chiu HF, Leung T, Lam LC et al. Sleep problems in Chinese elderly in Hong Kong. Sleep 1999;22:717-26.
- Blazer DG, Hays JC, Foley DJ. Sleep complaints in older adults: a racial comparison. J Gerontol A Biol Sci Med Sci 1995; 50:M280-4.
- Bixler EO, Kales A, Soldatos CR et al. Prevalence of sleep disorders in the Los Angeles metropolitan area. Am J Psychiatry 1979;136:1257-62.
- Gislason T, Almqvist M. Somatic diseases and sleep complaints: an epidemiological study of 3201 Swedish men. Acta Med Scand 1987;221:475-81.
- Klink M, Quan SF. Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest 1987;91:540-6.
- Sutton DA, Moldofsky H, Badley EM. Insomnia and health problems in Canadians. Sleep 2001;24:665-70.
- Hagen KB, Kvien TK, Bjørndal A. Musculoskeletal pain and quality of life in patients with noninflammatory joint pain compared to rheumatoid arthritis: a population survey. J Rheumatol 1997;24:1703-9.
- Andersson HI, Ejlertsson G, Leden I et al. Impact of chronic pain on health care seeking, self care, and medication. Results from a population-based Swedish study. J Epidemiol Community Health 1999;53:503-9.
- Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med 2002;251:207-16.
- Foley DJ, Monjan A, Simonsick EM et al. Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6800 persons over three years. Sleep 1999;22(Suppl 2)366-72.
- Falger PR, Schouten EG, Appels AW et al. Sleep complaints, behavioral characteristics and vital exhaustion in myocardial infraction cases. Psychology and Health 1988;2:231-58.
- Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol 1992;135:854-64. [AU: Please confirm that this is the correct reference. - Yes correct reference]
- Koskenvuo M, Kaprio J, Lönnqvist J, Sarna S. Social factors and the gender difference in mortality. Soc Sci Med. 1986;23(6):605-609. [AU: Please provide full reference.]
- Schwartz SW, Cornoni-Huntley J, Cole SR et al. Are sleep complaints an independent risk factor for myocardial infarction? Ann Epidemiol 1998;8:384-92. [AU: Please confirm that this is the correct reference.- Yes correct reference]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989;262:1479-84. [AU: Please confirm that this is the correct reference. - Yes correct reference]
- Breslau N, Roth T, Rosenthal L et al. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 1996;39:411-8.
- Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res 2002;53:561-9.
- Roberts RE, Shema SJ, Kaplan GA. Sleep complaints and depression in an aging cohort: a prospective perspective. Am J Psychiatry 2000;157:81-8.
- Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res 2006;40:700-8.
- Leger D, Guilleminault C, Dreyfus JP et al. Prevalence of insomnia in a survey of 12,778 adults in France. J Sleep Res 2000;9:35-42.
- Connor J, Norton R, Ameratunga S et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ 2002;324:1125.
- McCartt AT, Ribner SA, Pack AI et al. The scope and nature of the drowsy driving problem in New York State. Accid Anal Prev 1996;28:511-7.
- Fitzpatrick P, Kirke PN, Daly L et al. Predictors of first hip fracture and mortality post fracture in older women. Ir J Med Sci 2001;170:49-53.
- Brassington GS, King AC, Bliwise DL. Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64-99 years. J Am Geriatr Soc 2000;48:1234-40.
- Méndez Rubio JI, Zunzunegui MV, Béland F. The prevalence of and factors associated with falls in older persons living in the community. Med Clin (Barc) 1997;108:128-32.
- Akerstedt T, Knutsson A, Westerholm P et al. Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res 2002;53:741-8.
- Ohayon MM. Epidemiology of excessive daytime sleepiness. Sleep Med Clin 2006;1:9-16.
- Hublin C, Kaprio J, Partinen M. Daytime sleepiness in an adult, Finnish population. J Intern Med 1996;239:417-23.
- Ohayon MM, Caulet M, Philip P et al. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med 1997;157:2645-52.
- Nugent AM, Gleadhill I, McCrum E et al. Sleep complaints and risk factors for EDSin adult males in Northern Ireland. J Sleep Res 2001;10:69-74.
- Bixler EO, Vgontzas AN, Lin HM et al. EDS in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 2005;90:4510-5.
- Hasler G, Buysse DJ, Gamma A J. EDS in young adults: a 20-year prospective community study. J Clin Psychiatry. 2005;66:521-9.
- Tandberg E, Larsen JP, Karlsen K. Execssive daytime sleepiness and sleep benefit in Parkinson's disease: a community-based study. Mov Disord 1999;14:9227.
- Hobson DE, Lang AE, Martin WR. Excessive daytime sleepiness and sudden-onset sleep in Parkinson disease: a survey by the Canadian Movement Disorders Group. JAMA 2002;287:455-63.
- Kumar S, Bhatia M, Behari M. Excessive daytime sleepiness in Parkinson's disease as assessed by Epworth Sleepiness Scale (ESS). Sleep Med 2003;4:339-42.
- Bonanni E, Maestri M, Tognoni G et al. Daytime sleepiness in mild and moderate Alzheimer's disease and its relationship with cognitive impairment. J Sleep Res 2005;14:311-7. [Please confirm that this is the correct reference - Yes, reference is correct]
- Janson C, Gislason T, De Backer W et al. Daytime sleepiness, snoring and gastro-oesophageal reflux amongst young adults in three European countries. J Intern Med 1995;237:277-285.
- Foley D, Monjan A, Masaki K . Daytime sleepiness is associated with 3-year incident dementia and cognitive decline in older Japanese-American men. J Am Geriatr Soc 2001;49:1628-32
- Ohayon MM, Vecchierini MF. Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med 2002;162:201-8. [AU: Please confirm that this is the correct reference. - Yes, reference is correct]
- Hays JC, Blazer DG, Foley DJ. Risk of napping: EDS and mortality in an older community population. J Am Geriatr Soc 1996;44:693-8.
- Rockwood K, Davis HS, Merry HR et al. Sleep disturbances and mortality: results from the Canadian Study of Health and Aging. J Am Geriatr Soc 2001;49:639-41.
- Lyznicki JM, Doege TC, Davis RM et al. Sleepiness, driving, and motor vehicle crashes. Council on Scientific Affairs, American Medical Association. JAMA. 1998;279:1908-13.
- Garbarino S, Nobili L, Beelke M et al. The contributing role of sleepiness in highway vehicle accidents. Sleep 2001;24:203-6
- Howard ME, Desai AV, Grunstein RR. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med 2004;170:1014-21.
- Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev. 2008;12:129-41.